
Every doctor will encounter a lot of abbreviations in his study and work. If we can flexibly use these abbreviations to record medical records or review patients, we will not only greatly save time and energy, but also make writing more direct and concise.
More importantly, it is stipulated in the “Basic Standards for Medical Record Writing” that “medical records shall be written in Chinese, and common abbreviations in foreign languages and symptoms, signs and disease names without official Chinese translation can be written in foreign languages.”
Therefore, abbreviations must be standardized and cannot be misused. More attention should be paid to the long-term medical records stored in the input system.
Abbreviations are so common, do they all mean what?
Generally speaking, abbreviations are abbreviations composed of the first letters of each word, which is easier to remember.
For example, when asking for medical history and medical examination,
CC Indicates Chief Complaint
HPI indicates current medical history
PMH denotes past history
ALL indicates a history of allergy
VS for vital signs
In the current medical history and past history, HTN, HLP, DM and CHF can be used if common diseases such as hypertension, hyperlipidemia, diabetes and congestive heart failure occur.
In prescriptions, abbreviations are what can be seen on every prescription. The first is the way of administration, PR is the transrectal administration. SL means sublingual administration, SQ is subcutaneous injection, IM is intramuscular injection, and IV is intravenous injection.
Everyone knows that PO means oral administration, and after [nothing] is added, NPO means fasting.
In terms of medication frequency, we often use qod, qd, bid, tid, qid, qh, etc. in qod, qd and qh, q means [each, every], qac means before each meal, pc means only after meals, hs means before going to bed. Amp, caps, gtt, liq, sol, supp, susp, tab, ung respectively refer to injections, capsules, drops, liquids, solutions, suppositories, suspensions, tablets and ointments.
Although the symptoms are thousands of people, how to use the abbreviation?
Symptoms mainly reflect the subjective feelings of patients. The words describing symptoms are very rich and there is no fixed form. If the initials are still taken, everyone will find that many symptoms have the same face. After writing them down, review them again. I’m afraid I can’t remember what clearly.
Therefore, symptoms with very high recognition can be abbreviated, such as SOB, [shortness of breath], HA, headache, DOE, [dyspnea on extinction], which means labor-induced dyspnea, for example, short of breath, for short breath, for short breath, for short breath, for short breath, for short breath, for short breath, for short breath, for short breath, for short breath, for short breath, for short breath, for short breath, for short breath.
Although some symptoms have a [public face], they appear together with other friends, such as [nausea, vomiting] and [nausea/vomiting], which are abbreviated as [N/V], and the sense of presence is much stronger than when they appear alone. Similarly, diarrhea/constipation can be expressed as [D/C], fever, chills and sweating can be expressed as [F/C/S].
Negative signs are also commonly used.
In medical history or physical examination, we will use fixed expressions to describe some important negative signs, which will be easier and easier to use abbreviations. For example:
NKDA, or [not known drug allergies], denies a history of drug allergy.
EOMI [extraocular movements intact] indicates normal eye movements.
PERRL indicates that bilateral pupil is equal and round, and there is reactive to light.
During lung auscultation, both lungs have clear breathing sounds, which can be expressed by [clear to auscultation bilaterally] and CTAB.
The main murmur of lung auscultation, wheezing/dry rales/wet rales, can be expressed as W/R/R, i.e. [wheezes/rhonchi/rales].
Bowel sounds are expressed by BS, while normal intestinal peristalsis can be abbreviated as NABS.
If there is no cardiac abnormality in the patient’s auscultation, we can write as follows: RRR, S1/S2 is normal, and there is no M/R/G.
M/R/G is [murmurs/rubs/gallops], which represents cardiac murmur/pericardial friction sound/galloping rhythm, while RRR, [regular rate and rhythm] corresponds to the description of normal and regular heart rate.
Draw a picture to make it more vivid.
In addition to abbreviations, we can also add patterns to medical records, which are not only more visual, but also bring vitality to boring words.
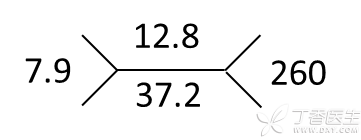
When expressing blood routine results, we can use Fig. 1 to represent more important data, representing leukocyte 7.9 × 109/L, hemoglobin 12.8 g/dL, hematocrit 37.2%, platelet 260 × 10 9/L, smart people can also use imagination, users similar methods to represent electrolyte and other test results.
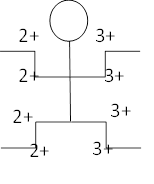
When doing tendon reflex, the little person in Fig. 2 shows biceps brachii tendon reflex, triceps brachii tendon reflex, knee tendon reflex and Achilles tendon reflex. The right side is normal and the left side is active. You can also add Babinski sign + or-to the foot.
However, it should be noted that these pictures are more suitable for use when making records. In medical records, formal language should still be used.
