
Finger pricking to measure blood sugar, subcutaneous injection of insulin, weight loss and lifelong medication can be called the [four nightmares] of sugar lovers.
In response, doctors and scientists have also used 18 kinds of martial arts to develop various new technologies and equipment.
Today, Dr. Clove will take a look at these new breakthroughs in the treatment of diabetes.
Non-invasive blood glucose monitoring
As we all know, monitoring blood sugar is a [compulsory course] for sugar lovers every day. Some sugar lovers need to monitor blood sugar 5 times or even 7 times a day. They can only shed tears silently when looking at their fingers with needles everywhere:
The pain of pricking fingers is only understood by me who needs to monitor blood sugar!
If only there were an artifact that could know the blood sugar level without pricking a finger!
The scientist replied:
This wish, we will satisfy you!
Now, scientists have developed a series of non-invasive blood sugar monitoring devices. These devices estimate blood sugar by monitoring changes in skin surface, glucose content in body fluid components, photoelectricity, etc.
Compared with traditional finger blood sugar monitoring, non-invasive blood sugar monitoring does not require pricking fingers and is more convenient and fast. For example, there are types designed as contact lenses, or types of bracelets and watches. These devices can provide all-weather blood sugar data.

However, they also have shortcomings.
For example, most non-invasive blood sugar monitoring equipment is expensive, and consumables should be replaced regularly and calibrated according to finger blood sugar.
At present, the United States and Europe have approved several non-invasive blood sugar monitoring devices to be sold on the market, but these devices are very vulnerable to external interference. For example, devices monitoring blood sugar through contact lenses may not read correctly when the wearer shed tears. Blood sugar monitoring equipment such as bracelets and watches are easily interfered by sweat and temperature changes on the skin surface, resulting in inaccurate blood sugar data.
Therefore, until these devices solve the above problems, clinicians still do not recommend sugar lovers to blindly use non-invasive blood glucose monitoring devices for blood glucose monitoring.
Tie your finger every day, how doesn’t hurt? Click: 7 Tips for Pricking Fingers Without Pain
Dynamic blood glucose monitoring
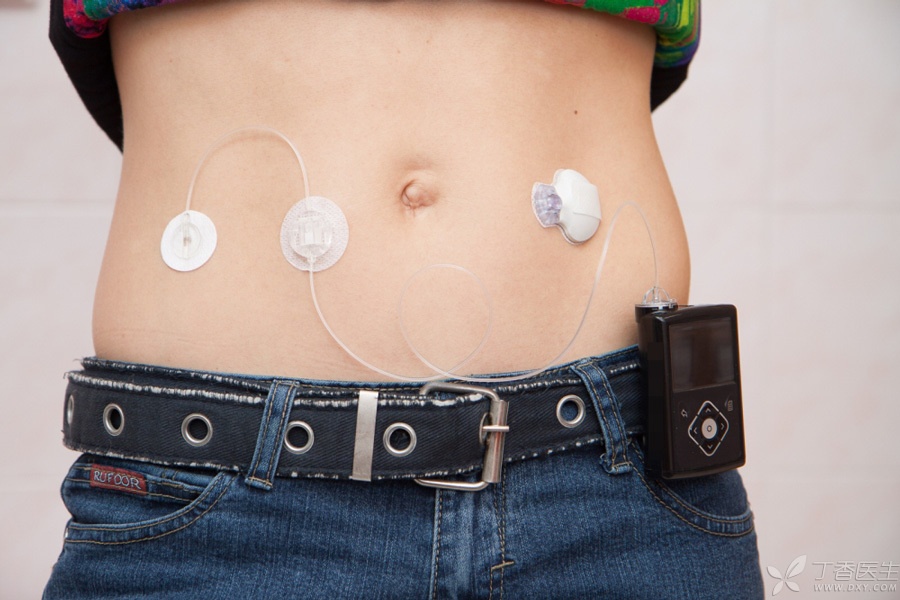
For sugar lovers with large blood sugar fluctuation or frequent blood sugar measurement, especially patients with type 1 diabetes, clinicians may recommend the use of dynamic blood sugar monitoring equipment.
It monitors the glucose concentration in the surrounding tissue fluid through a probe implanted subcutaneously to indirectly calculate the blood sugar value. This probe is very thin and can be safely implanted subcutaneously for several days without causing discomfort, affecting daily life and even swimming with it.
Dynamic blood glucose monitoring is a mature technology, and the accuracy of the equipment is no less than that of traditional fingertip blood glucose monitoring. However, its price is relatively high. To replace the probe and calibrate regularly, it needs to be used under the guidance of doctors.
Inhaled insulin
For sugar lovers who want to inject insulin, pricking their skin every day and injecting insulin often requires some psychological construction. Inhaled insulin can solve sugar lovers’ fear of needles.
Inhaled insulin stores dry insulin powder in a separate package and needs to be used in conjunction with corresponding inhalation devices.
When in use, the dry insulin powder forms a spray in the inhalation device. After the sugar friend inhales the lungs, the dry powder dissolves immediately, and the released insulin can quickly enter the blood to play a role.
At present, the United States has approved the listing of an inhaled insulin, but there is no domestic listing of inhaled insulin.

Inhalation of insulin may cause respiratory discomfort such as cough, so patients with respiratory diseases such as asthma, chronic bronchitis and emphysema cannot use it.
At present, there are only 4 units and 8 units of two packages for inhaling insulin, which need to be inhaled repeatedly when increasing the dose, and it is not convenient to adjust the dose. In addition, the price of inhaling insulin is high, and the acceptance and satisfaction of users to inhaling insulin do not exceed that of injecting insulin. Therefore, doctors still recommend sugar lovers to choose traditional injecting insulin.
Only by mastering the correct injection method of insulin can the pain be reduced. Click: Standardize insulin injection to reduce injection pain
Bariatric surgery
The purpose of bariatric surgery is to transform the original [King of Big Stomach] into [Bird Stomach], which will naturally help people lose weight after eating less.
In addition, for obese patients with type 2 diabetes who have poor weight loss effect, weight loss surgery is a good news for improving blood sugar.
In our country, for those aged between 18 and 60, In good health, The risk of surgery is low, For type 2 diabetes patients with BMI ≥ 32 kg/m2, when it is still difficult to control blood sugar by hypoglycemic therapy on the basis of diet control and exercise, doctors may consider bariatric surgery. For type 2 diabetes patients with BMI not reaching 32 kg/m2, if judged by doctors, bariatric surgery can be performed, or bariatric surgery may be adopted after careful evaluation of the disease condition.
The most common and preferred method in bariatric surgery is [laparoscopic sleeve gastrectomy].
As shown in Figure 1, about 80% of the stomach is removed through surgery, leaving a tubular gastric passage, thus reducing appetite.
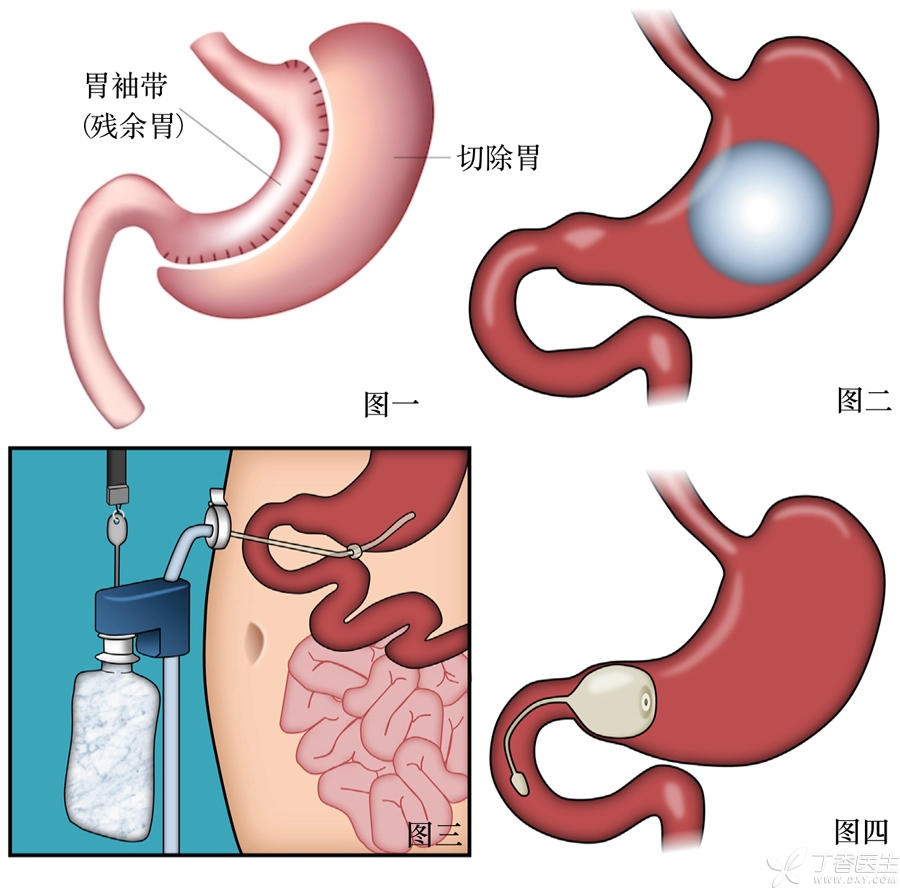
In order to avoid the risks of traditional weight loss surgery, doctors have also developed some very imaginative minimally invasive weight loss surgery methods.
Some operations use inflatable balloons (Fig. 2) to occupy a part of the stomach volume, thus making patients feel full when eating less, thus reducing appetite.
There is a weight loss device that has been approved for listing in the United States (Fig. 3). Doctors install a pipe in the patient’s abdomen to lead to the stomach, and then through a suction device, part of the food in the stomach can be extracted, thus reducing the amount of food absorbed.
Other operations (Fig. 4) install a delay device at the gastrointestinal junction to delay the speed of gastric emptying, which also plays a role in increasing satiety and reducing appetite.
Here need to remind everyone, bariatric surgery is not once and for all, still need to adhere to healthy diet, reasonable exercise and hypoglycemic treatment after surgery. Moreover, the operation also has the possibility of complications such as bleeding, poor healing, etc. In the long run, the operation also has the risk of causing nutritional deficiency, cholelithiasis and other diseases.
Therefore, if you consider undergoing bariatric surgery, you need to go to a qualified hospital and consult a doctor before making a decision.
Pancreas/islet transplantation
Pancreas/islet transplantation is mainly aimed at patients with type 1 diabetes who are difficult to control blood sugar and prone to hypoglycemia. Transplantation can rebuild the normal mechanism of blood sugar regulation, effectively prevent the occurrence of severe hypoglycemia and delay the occurrence and development of diabetic complications.
Pancreatic transplantation is a kind of organ transplantation. If the pancreatic transplantation is successful, the patient can even get rid of insulin. Currently, there are about 1,000 pancreatic transplants performed in the United States every year, most of which are patients with end-stage diabetic nephropathy who need kidney transplantation, and pancreatic transplantation is performed at the same time.
Islet transplantation is to inject purified islet cells into the liver of the transplanted patient through a transcutaneous catheter needle. In contrast, islet transplantation is less traumatic. Islet transplantation can effectively reduce the occurrence of severe hypoglycemia, reduce the use of exogenous insulin and improve blood sugar control after islet transplantation.
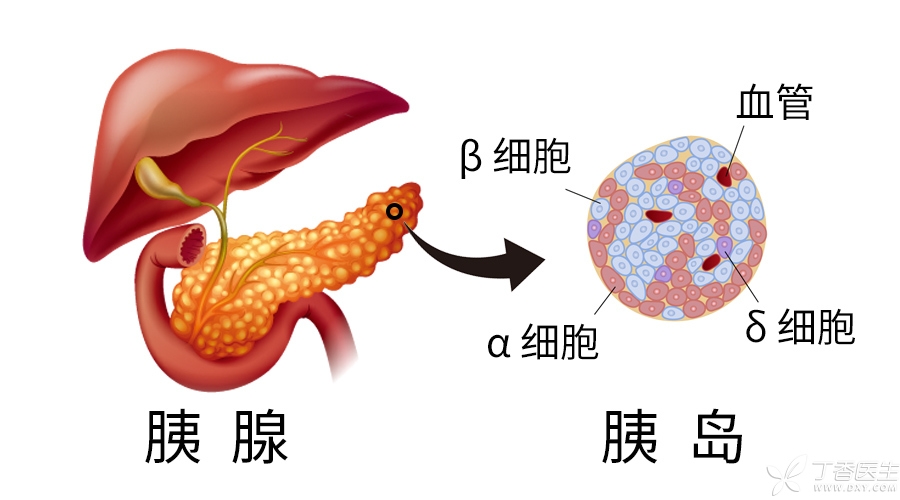
However, receiving pancreas/islet transplantation does not mean that diabetes treatment is once and for all.
After pancreas/islet transplantation, patients need to take immunosuppressive drugs for life.
In addition, the long-term effect of islet transplantation is not as good as that of pancreatic transplantation, and the death of transplanted islet cells is easy to occur within a few years after transplantation. In addition, the collection of islet cells is relatively difficult. During islet transplantation, the pancreas of six organ donors needs to be collected to meet the islet cells needed by one patient for islet transplantation.
Under the condition of continuous blood sugar monitoring or insulin pump, some doctors think pancreas/islet transplantation can be considered when hypoglycemia still occurs frequently in patients with type 1 diabetes or when blood sugar in patients with type 2 diabetes is still difficult to control.
However, due to organ shortage, large trauma of pancreatic transplantation and poor long-term effect of islet transplantation, pancreatic/islet transplantation still has a long way to go as a routine therapy to control blood sugar.
Stem cell therapy
Stem cells, unlike ordinary cells, can differentiate into other cells. Using this characteristic of stem cells, stem cells can differentiate into islet cells.
In theory, stem cells have the possibility of curing type 1 diabetes. Because stem cells can redifferentiate to produce insulin-secreting cells and protect patients’ islet cells from attacks by the autoimmune system, they are indeed the hope of curing insulin-deficient type 1 diabetes.

However, most of the research on stem cell therapy is still at the effective stage of in vitro experiments, and there are still many potential safety problems in stem cell therapy for diabetes.
For example, animal experiments have shown that stem cells transplanted into the body may produce mutations, leading to the occurrence of tumors. In addition, immune rejection may still occur after stem cell transplantation, requiring lifelong use of immunosuppressants.
Therefore, whether stem cell therapy can safely and effectively rebuild normal glucose metabolism still needs to wait for more clinical trial results to be determined.
There are some intermediary companies on the Internet, It is said that it can help diabetics go abroad and receive the so-called advanced stem cell therapy. Here we need to remind everyone that the technology of stem cell therapy for diabetes is not yet mature and many problems have not been solved. It is not a safe and effective method. We must not try our best to take risks. It does not count as a waste of money, but also delays formal treatment and leads to a series of future troubles.

What should we do now?
Although many of these technologies are in the research and development stage and are not yet mature, they also ignite the light of hope for curing diabetes.
Now sugar friends should do, and everyone can do, is to shut up, take your legs, use good medicine, do a good job of blood sugar monitoring, with a peaceful mind and diabetes [peaceful coexistence].
Sugar friends are their own diabetes treatment drivers. In addition to their daily work and life, they drive diabetes self-management vehicles: diet, exercise and drugs are engines, self-test blood sugar is headlights, and continuous learning of diabetes self-management related knowledge is gasoline.
Dr. Clove, willing to do everyone’s diabetes knowledge [gas station], on the way to fight sugar, and everyone forward.
