Are you going to have an operation? Please have a heart consultation first… … …
The incidence and mortality of non-cardiac surgery-related complications worldwide are 7% ~ 11% and 0.8% ~ 1.5% respectively every year, of which 42% are cardiac complications. How to assess cardiovascular risks before surgery is a common clinical problem and a common worry for doctors in surgical departments and cardiovascular doctors.
Operators (surgery, obstetrics and gynecology, otolaryngology, oral cavity, ophthalmology, etc.) are worried about whether the operation can be performed and the risks, especially for patients with previous history of cardiovascular diseases or abnormal ECG and cardiac color Doppler ultrasound.
Physicians, on the other hand, are distressed by how to objectively evaluate risks. In the current [tense] medical environment, they will neither avoid nor assume too many [responsibilities].
European < < 2014 ESC/ESA Guidelines for Non-Cardiac Surgery: Cardiovascular assessment and management > > and < < 2014 ACC/AHA Guidelines for Perioperative Cardiovascular Assessment and Treatment for Non-cardiac Surgery > > in the United States put forward detailed strategies for objectively evaluating and managing cardiovascular risks before surgery. However, the guidelines in Europe and the United States also have [acclimatization] places in China, which need to be adjusted in combination with domestic reality.
Selective surgery should be postponed under the following circumstances
Combined with the following cardiovascular instability, first see if it is an emergency operation, if it is not an emergency operation, should consider postponing, first deal with heart problems. According to the guidelines, the author integrates the following three points:
-
Acute coronary syndrome (ACS)
-
Acute heart failure
-
Symptomatic severe aortic stenosis, severe mitral stenosis with pulmonary hypertension
So, how to deal with it? Can what consider surgery?
-
After ACS revascularization, the operation should best be delayed to 14 days after balloon dilation, 30 days after metal bare stent implantation and 1 year after drug stent implantation. However, if the second generation drug stent is implanted, the waiting time can be shortened to 3-6 months after evaluating the risks and benefits.
-
Acute heart failure, stable heart function 3 months later surgery.
-
Symptomatic severe aortic valve stenosis is recommended to be replaced first. If biological valve is replaced, warfarin anticoagulation is required for 6 months. For severe mitral stenosis complicated with pulmonary hypertension, percutaneous mitral valvuloplasty may be considered first.
It should be noted that cardiovascular instability does not include:
-
Stable coronary heart disease. For coronary heart disease, it mainly depends on whether it is stable, not the degree of vascular stenosis.
-
Stable phase of chronic heart failure is not included in this category. Elective surgery may be considered.
-
In valvular diseases, attention should be paid to the simultaneous existence of the key words [symptomatic] [severe] [stenosis]. Other valvular heart diseases (aortic insufficiency and mitral insufficiency) are not included in this category. Surgery may be considered.
After investigating cardiovascular instability, it is shown that surgery can be done, and the next step is to assess risks and control risks.
Metabolic equivalent (MET) is an important indicator
The most important tool for preoperative cardiovascular risk assessment is not electrocardiogram, cardiac color Doppler ultrasound or coronary CTA, but metabolic equivalent (MET), an indicator that can be obtained simply through medical history inquiry.
Metabolic equivalent is an important indicator of relative exercise intensity, which simply reflects the patient’s activity tolerance. It is divided into 1 to 10 grades, 1 MET represents dressing, eating and other activities, 4 METs represents climbing 2 flights of stairs, and 10 METs represents playing ball, swimming, climbing and other activities.
The United States guidelines recommend that:
Patients with increased risk of adverse cardiac events (MACE) but excellent metabolic equivalents (> 10 METs) can undergo surgery (IIa, B) without further exercise tests and cardiac imaging examination. MACE may be reasonable for patients with increased risk but moderate to good metabolic equivalents (4 ≤ METs < 10) without further exercise tests and cardiac imaging examination and surgery (IIb, B).
There are similar recommendations in the European guidelines.
Therefore, after examining the cardiovascular instability mentioned above, patients should be asked three key questions before operation:
Can I take care of myself?
Will you have asthma and chest tightness on the 2nd floor of stairs?
Do what sports at ordinary times?
According to European and American guidelines, even for patients with high cardiovascular risks, if the patient can easily climb more than two floors and has an activity tolerance greater than 4 METs, the examination does not need to be done more and surgery can be performed.
Quantitative risk assessment: NSQIP, RCRI
Quantitative evaluation tools have the advantages of being objective, but the disadvantages are cumbersome and inconvenient to use. Clinicians cannot remember the risk scoring standards one by one. So, how do what need to calculate these cumbersome scores?
As mentioned above, it is recommended to postpone non-emergency surgery for cardiovascular instability. If metabolic equivalent ≥ 4 METs, even patients with increased MACE risk can consider surgery. So, what should we do when metabolic equivalent < 4 METs? At this time, quantitative risk assessment (NSQIP, RCRI) is needed.
National Surgical Quality Improvement Program ( NSQIP) Can be used to assess the risk of surgical complications ( Scan the two-dimensional code below to enter the website). Enter the operation name (judging high school and low risk surgery), age, sex, mobility, hormone use history, whether there is ascites within 30 days, whether there is septicemia, mechanical ventilation, tumor metastasis, diabetes, hypertension, COPD, heart failure, dyspnea, smoking, dialysis, acute renal failure, height, weight and other parameters within 48 hours. In addition to cardiovascular risks, objective quantitative risks of a series of complications (pulmonary infection, urinary tract infection, deep vein thrombosis, renal failure, etc.) can be obtained.

The risk classification of the operation itself is the main influencing factor. It should be noted that the risk of the operation is definitely not distinguished by [local anesthesia] [spinal anesthesia] [general anesthesia], but the operation itself. Occasionally, I will receive a consultation form to write [general anesthesia surgery], but I will not mention what surgery at all. Such doctors have a biased understanding of the operation risk.
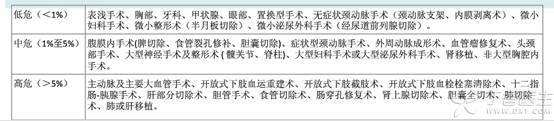
It can be seen that common operations such as thyroid gland, ophthalmology and prostate resection are classified as low-risk operations. The guidelines mention that if patients undergo low-risk operations (such as ophthalmic operations), even if there are various cardiovascular risk factors, the risk of serious adverse events during the operation is very low. If the patient undergoes macrovascular surgery, even if the coexisting cardiovascular risk factors are very few, the risk of serious adverse events during surgery is still high.
The revised cardiac risk index (RCRI) is an off-line evaluation method, involving 6 predictive factors: creatinine ≥ 2 mg/dl, heart failure, insulin-dependent diabetes mellitus, transthoracic, abdominal surgery or large vessel surgery above groin, previous stroke or transient ischemic attack, ischemic heart disease; 0 ~ 1 predictive factor is low risk, ≥ 2 predictive factors are higher risk.
What should patients with high cardiovascular risks do after NSQIP and RCRI scores? The author summarizes three main points:
-
Multidisciplinary consultation
-
Fully perfect the inspection
-
Fully explain risks to patients
At this point in the process, It is not an individual or a single subject that can decide the treatment plan. Multidisciplinary consultation is required. Including surgical departments, cardiology departments, anesthesiology departments and related departments, Formulate the best plan and share the risks. Then fully improve the relevant examinations: including electrocardiogram, cardiac color Doppler ultrasound, drug load test, coronary CTA, and even coronary angiography. According to the calculated and discussed results, fully communicate the risks with patients and their families and jointly decide whether to operate now or postpone the operation.
Risk management of various cardiovascular diseases
Coronary heart disease
Coronary heart disease is the most common complication, and the treatment has the following details. This refers specifically to stable coronary heart disease. ACS has been discussed above, and revascularization is recommended first.
1. Do you need revascularization first
The guidelines suggest that stable coronary heart disease generally does not consider revascularization first. Unless high-risk coronary heart disease patients undergo high-risk surgery (IIb, B).
So what is high-risk coronary heart disease? According to the European < < 2013 ESC Guidelines for the Management of Stable Coronary Artery Diseases > >, it can be simply defined as obvious left main lesion, three-branch lesion and anterior descending branch proximal lesion.
Therefore, for example, if the patient intends to undergo partial hepatectomy (high-risk surgery), such as coronary artery is three-branch lesion, or left main trunk stenosis is more than 50%, anterior descending branch proximal stenosis is more than 70%, revascularization (PCI or CABG) can be considered, which is a Class IIb recommendation. If it is only a single branch lesion of circumflex branch or right crown, etc., no matter how severe the stenosis is, revascularization is not recommended first.
Methods of revascularization include balloon dilatation (14 days delay), bare metal stent implantation (30 days) and drug stent implantation (1 year). If the second generation drug stent is implanted, the waiting time can be shortened to 3-6 months after evaluating the risks and benefits. CABG may be considered if the operation is to be carried out as soon as possible and the lesion is not suitable for using bare stent.
2. Regulation of antiplatelet drug
Another key issue in the adjustment of antiplatelet drugs is how to stop using them before operation and how to resume using them after operation.
Aspirin is recommended to be stopped for 7 to 10 days before operation, tigrilol and clopidogrel are recommended to be stopped for 5 days. According to the risk of hemorrhage after operation, it is best to resume the use of antiplatelet drugs as soon as possible after 24 to 48 hours, and one can be recovered first.
During the discontinuation of antiplatelet drugs, the use of low molecular weight heparin bridging has proved ineffective and may also increase the risk of surgical bleeding.
3. Perioperative management
The guidelines recommend that troponin should be checked before and 48 ~ 72 hours after high-risk coronary heart disease.
In addition, attention should be paid to the presence or absence of chest tightness, chest pain, cold sweat and other myocardial ischemia symptoms. Intraoperative and postoperative coronary artery perfusion insufficiency caused by hypotension should be avoided. In terms of drugs, secondary prevention drugs for coronary heart disease such as ACEI/ARB and statins should continue to be used. It is also recommended to use receptor blockers in patients with high ischemia risk and recover antiplatelet drugs as soon as possible.
Atrial fibrillation
Atrial fibrillation is mainly related to anticoagulation. Patients who use warfarin for anticoagulation should stop using warfarin and switch to low molecular weight heparin for anticoagulation, then stop using warfarin once 12 hours before operation, and resume using low molecular weight heparin and warfarin after operation according to the risk of hemorrhage.
Heart failure
Perioperative management:
Attention should be paid to the amount of entry and exit, control the amount and speed of entry (usually 1 ml/kg/h), and pay attention to the symptoms of aggravation of heart failure such as heart rate increase, shortness of breath, and increased rales in the lungs. Pro-NT-BNP or BNP should be detected with cardiotonic and diuretic drugs to adjust the cardiac function to a better state.
Drugs:
Continue to optimize the use of ACEI/ARB, receptor blockers, aldosterone receptor antagonists and other drugs to improve the prognosis of heart failure. It should be noted that unless the receptor blockers have sufficient titration time, it is not recommended to use large doses of receptor blockers before operation, because it may aggravate heart failure in the short term.
Hypertension
Control Objectives:
The guidelines recommend that systolic blood pressure < 180 mmHg and diastolic blood pressure < 110 mmHg do not delay the operation time (IIb, b). However, if there is sufficient time for elective surgery, the adjustment target is below 140/90 mmHg.
Inducement of blood pressure rise during perioperative period:
Surgical tension and anxiety, surgical incision pain, hypoxia, excessive fluid intake, intestinal flatulence, urine retention, nausea, vomiting, etc. Preoperative blood pressure control can be achieved, and postoperative blood pressure is significantly increased, the inducement needs to be eliminated.
Drug selection:
Antihypertensive drugs with quick effect can be selected, and surgery can be performed as soon as the blood pressure reaches the standard, such as CCB nifedipine sustained-release agent. Patients with systolic blood pressure above 160 mmHg can start to use ACEI/ARB together. Diuretics should be cautious because they will aggravate the loss of body fluids related to surgery.
Valvular disease
In addition to symptomatic severe aortic stenosis and mitral stenosis complicated with pulmonary hypertension, valve treatment is required before surgery.
Severe mitral regurgitation and severe aortic regurgitation, such as stable cardiac function, are feasible for surgery (IIa, C). However, asymptomatic severe aortic stenosis and severe mitral stenosis need to assess the risks and benefits and decide whether to treat the valve first.
Patients undergoing biological valve replacement need anticoagulation for half a year, while patients with mechanical valve need anticoagulation for life. Therefore, biological valve should be selected for cardiac surgery. If surgery is required during anticoagulation, warfarin can be stopped and low molecular weight heparin bridging can be used instead.
Arrhythmia
Frequent ventricular premature does not affect the operation.
If there is ventricular tachycardia, please consult the cardiovascular internal medicine department to judge whether it is idiopathic ventricular tachycardia. If it is idiopathic ventricular tachycardia, the risk related to surgery is small, and the author can give antiarrhythmic drugs (lidocaine and codarone) for repeated occurrence.
Perioperative bradycardia is common, especially after anesthesia. Attention should be paid to reexamination of electrolytes.
Pay attention to ask whether there are symptoms of syncope, blackness and dizziness in the past and now, whether the blood pressure is normal, and give ECG monitoring to observe whether there is a long R-R interval of more than 3 seconds. If there is any, temporary pacemaker can be considered. If there are no symptoms, the blood pressure is normal, and the heart rate is less than 40 bpm, atropine or isoproterenol can be temporarily used to increase the heart rate.
5. Adjust the strategy according to the actual situation in China
The guidelines in Europe and the United States are well-founded. However, it is also necessary to combine the domestic reality. Some recommendations are difficult to implement in China, such as:
1. In the guidelines, for asymptomatic patients undergoing low-risk surgery, routine resting 12-lead electrocardiogram (III, B) is not required.
All patients in China are routinely examined by electrocardiogram. Although angina pectoris and myocardial infarction are low probability events after operation, in case of occurrence and medical disputes, even a 20-dollar electrocardiogram was not done before operation, which is hard to say.
2. In the guidelines, color Doppler ultrasound is recommended only if there is dyspnea for unknown reasons, or if there is heart failure that has not been reexamined for one year or if dyspnea is aggravated. Routine cardiac color Doppler ultrasound (III, B) is not recommended.
U.S. Color Doppler ultrasound to 5 000 RMB at a time. And in China about 300 yuan. In fact, the indications of cardiac color Doppler ultrasound are far from so strict. In the past, when there are heart diseases or electrocardiogram changes that are difficult to analyze, cardiac color Doppler ultrasound can be further evaluated. Highly suspected coronary heart disease, coronary CTA or coronary angiography is feasible for clear diagnosis.
3. Whether to stop aspirin before operation needs to measure the risk of hemorrhage and embolism. For patients who are receiving aspirin therapy and are accompanied by medium-risk or high-risk factors of thromboembolism, if non-cardiac surgery is to be performed, it is recommended to continue taking aspirin during the operation.
It is not feasible to use aspirin continuously before operation in China for most of the time. First of all, most surgeons have no experience in performing operations on the basis of taking aspirin and are afraid of bleeding. Second, not many physicians are willing to take this risk. In case of massive bleeding during operation, how can they say clearly that it is not the cause of aspirin?
In a word, for cardiovascular risk assessment before surgery, cardiovascular instability (ACS, acute heart failure, symptomatic aortic stenosis) should be investigated first, MET should be evaluated, and risk quantitative score (NSQIP, RCRI) should be calculated when necessary. While referring to European and American guidelines, domestic reality should be considered. Surgery should be done well and risks should be managed well.
Author: Mai Jingting, Department of Cardiovascular Internal Medicine, Sun Yat-sen Memorial Hospital, Sun Yat-sen University.
Source: www.hizy.net Genuine Photo Library/Author Provided
