
Editor’s Note: Feng Yibing, co-author of this article, is a doctor at Yuetan Community Health Service Center, Fuxing Hospital Affiliated to Capital Medical University.
With the continuous growth of the number of HIV-infected people, previous HIV-infected people have also entered the onset period one after another, and the demand for health services among this population has also increased dramatically.
As a doctor, Of course, it is to keep one’s promise. Take the patient’s health as the first consideration and do everything possible to treat the patient. More and more news reports [XX Hospital refuses to admit AIDS patients and doctors discriminate against HIV/AIDS] attract people. Whenever similar reports appear, hospitals and medical personnel are accused of [prevarication], [discrimination] against patients, and even being abused for not having medical ethics, etc.
As medical workers, who should we tell to when we bear so many grievances and how should we avoid the risks we bear clinically as much as possible?
Today, Clove Garden invited Director Wang Lu of the Propaganda Department of the Sex AIDS Center of the China Center for Disease Control and Prevention, who is fighting in the frontline of AIDS prevention, and Dr. Feng Yibing of the Yuetan Community Health Service Center of Fuxing Hospital Affiliated to Capital Medical University, to tell everyone how to protect themselves from the threat of AIDS to the greatest extent in clinical practice.
First, there is no need to be afraid of needle stabbing, which is not necessarily contagious.
Occupational exposure is the most worrying problem.
AIDS incubation period paid, HIV-infected people are unrecognizable on the outside, In the course of work, Often come into contact with the patient’s body surface, wounds, semen, vaginal secretions, etc. Therefore, medical workers, especially surgeons, stomatologists, obstetricians and gynecologists, staff caring for HIV infected persons and AIDS patients, relevant blood banks, laboratory and hemodialysis ward staff and autopsy personnel, etc., are always exposed to the risk of HIV infection.
However, needle stabbing does not necessarily lead to HIV infection. The premise, of course, depends on whether the needle is contaminated with HIV. If the needle is contaminated with HIV, for example, it is clear that the other party is infected with HIV, such worries can only be established. In addition, the following points should be paid attention to:
- The possibility of infection is related to the characteristics of the needle, the depth of the stab wound, whether there is visible blood on the needle and the amount of blood, the infection stage of the infected patient, and the genetic characteristics of the injured. Hollow needles are more likely to infect than solid needles. The deeper the stab wound, the more contaminated blood on the needle, and the greater the possibility of infection. If the patient who is the source of infection dies of AIDS within 2 months after being stabbed, the possibility of infection is high. Generally speaking, the average blood volume of acupuncture is 1.4 L, and the probability of HIV infection in one needle stab wound is 0.33%. (The risk probability of HIV occupational exposure investigated in the United States is about 6.4/10,000, which is significantly lower than the 19% infection probability of medical personnel exposed to hepatitis B virus stab wound).
Second, different departments have different protection points
We have already prepared articles for you in different specialties. Click here to see how different departments should protect AIDS.
Three, really be needle stuck to how to do?
Of course, we should avoid occupational exposure to HIV as much as possible, but even if we are careful, there will be misfortune or accidents. How should we protect ourselves?
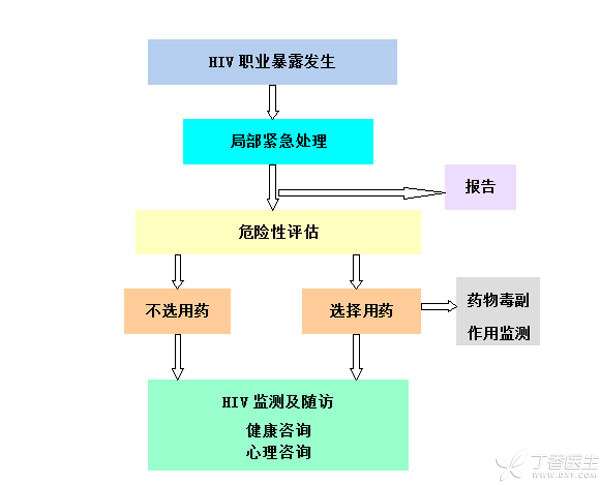
Treatment Process after Occupational Exposure to HIV
Please remember: one squeeze, two washes and three disinfections, while evaluating and reporting.
One squeeze, two washes and three disinfection:
It is about local treatment after exposure:
-
If blood and body fluids are splashed on the surface of skin and mucosa, soap should be used immediately, then clear water, tap water or normal saline should be used for rinsing.
-
If it splashes into oral cavity, eyes and other parts, rinse thoroughly with clear water, tap water or normal saline for a long time.
-
In case of hemorrhagic injuries such as skin and mucosa needle injury, cutting injury and bite injury, the blood of the injured part should be extruded immediately, then thoroughly washed with clear water, tap water or normal saline, etc., and then the wound surface should be disinfected with iodophor, 75% alcohol, 0.2% sodium hypochlorite, 0.2% ~ 0.5% peracetic acid, 3% hydrogen peroxide, etc.
While evaluating, report:
The assessment and treatment should be done by specially trained and experienced AIDS experts.
The following passage is very important to everyone, please keep in mind:
After medical personnel are contaminated by blood or other body fluids containing HIV, in addition to wound disinfection and treatment, they can choose to take drugs according to the situation to prevent the occurrence of HIV infection. Drug prevention has been proved to reduce the occurrence of HIV infection after needle stab injury, so there are drugs that can prevent occupational exposure.
However, it should be noted that if antiviral drugs are needed, the faster the time limit is, the better. Generally, the preventive effect of taking drugs within one hour is the best.
Therefore, in the event of unfortunate occupational exposure, the local Center for Disease Control and Prevention must be notified as soon as possible to report and request experts to evaluate and claim necessary antiviral drugs, so as to control the infection as much as possible.
Four, actively promote the national protection policy for medical personnel
If medical staff have to go out to receive patients regardless of their lives, then the state should also have the obligation to protect medical staff regardless of their lives. However, the protection of medical staff by the state is far from sufficient.
Improving the medical treatment conditions for HIV/AIDS requires long-term efforts from many parties.
1. Patient diversion should be done well.
There are no independent infectious disease hospitals in developed countries abroad. Instead, patients with infectious diseases are treated in special areas of general hospitals. Such as tuberculosis, AIDS, hepatitis and so on. China should learn from this concept and bring the treatment of infectious diseases into the unified management of the conventional medical system. To build a perfect and in-place medical system for infectious diseases, specialized hospitals should not only be able to treat infectious diseases, but also have comprehensive medical capabilities. On the other hand, they should improve the prevention and treatment capabilities of infectious diseases in general hospitals.
2. Preoperative examination is indispensable
AIDS patients and infected persons have the right to treatment, and medical personnel also have the right to protection.
Due to the consideration of patients, medical care and hospitals, China’s “AIDS Management Regulations” stipulate that patients are routinely examined for hepatitis B, hepatitis C, syphilis and AIDS before undergoing surgery or invasive surgery.
Due to the protection of privacy, the United States does not carry out mandatory HIV tests on preoperative patients, but treats all patients according to the infection level. The treatment principle is based on the General Protection recommended by WHO.
3. Medical training should be sufficient.
Previous survey results show that many of our medical personnel have low awareness of universal protection principles, lack of protection knowledge, and lack of knowledge and skills for post-exposure treatment.
The government should strengthen the occupational protection knowledge training of medical personnel and enhance the awareness of prevention and control of medical personnel so as to reduce the occupational exposure to AIDS. At the same time, the government should improve the compensation mechanism for the staff engaged in infectious diseases while strengthening the occupational safety protection and safeguard measures for medical personnel.
