
What should be explained after lumbar puncture?
I believe the vast majority of people will answer: [Go to the pillow and lie down for 6 hours to avoid headache after operation], which is what textbooks have always said and what we have done. However, have you ever doubted this sentence?
Why [go to the pillow and lie down for 6 hours]?
Headache is the most common complication of lumbar puncture, which is related to cerebrospinal fluid leakage from dura mater caused by excessive puncture needle or vertical cutting of longitudinal fibers, excessive collection of disposable cerebrospinal fluid, etc.
The decrease of cerebrospinal fluid volume, on the one hand, makes cerebrovascular mechanical expansion and stimulates pain-sensitive tissues on the vascular wall to cause headache, on the other hand, makes the brain move down and traction cranial cavity pain-sensitive structures to cause headache [1].
Standing position or high pillow can induce or aggravate headache due to gravity. Therefore, it is recommended to remove pillow and lie down after operation.
However, evidence-based medicine does not say so.
On March 7 this year, Cochrane Library, a well-known evidence-based medicine database, published a systematic review of Posture and fluids for preventing post-dural puncture headache, summarizing 24 studies and analyzing the following conclusions:
We found low to modern quality event that bed rest does not prevent the onset of headaches after lumbar puncture, regardless of the duration of rest or the body or head positions assumed by the patient.
There is low to medium quality evidence that bed rest cannot prevent headache after lumbar puncture, regardless of duration or body position.
However, due to the limitation of experimental design methods, these studies are difficult to be double-blind, so the quality of evidence is low.
So, is it the same at home?
Some people will say that the test results cannot be directly adopted due to the different constitutions between the East and the West and the different lumbar puncture techniques or needle thicknesses, and our teaching materials shall still prevail.
In China, there are many similar tests:
Yang Lijuan et al. [2] have done such experiments: 300 patients with lumbar puncture were divided into 2 groups after operation. The control group was divided into 2 groups. The control group was divided into 2 groups. The control group was divided into 2 groups. The control group was divided into 2 groups. The control group was divided into 2 groups. The control group was divided into 2 groups. The control group was divided into 2 groups. The control group was divided into 2 groups. The control group was divided into 2 groups. The control group was divided into 2 groups.
In coma patients, the vital signs before and 2, 4, 6 hours after lumbar puncture and the observation of mind, pupil, vomiting and pressure ulcer were taken as observation items. Awake people take headache and comfort as observation items, and get the following results:
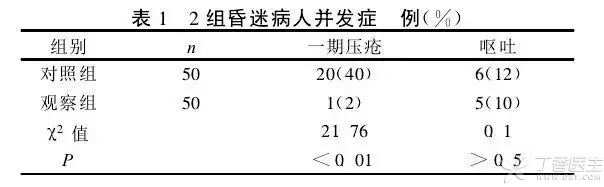

There was no significant difference in the incidence of vomiting between the two groups of coma patients, while the observation group with regular turn-over decreased the incidence of pressure ulcer due to relieving skin pressure for a long time, which was statistically significant. The comfort level of the observation group with low pillow for conscious patients was higher, but the incidence of headache did not increase.
Mikai et al. [3] once divided 90 cases after lumbar puncture into 30 cases in high intracranial pressure group, 30 cases in normal intracranial pressure group and 30 cases in low intracranial pressure group for observation, supplementing the problem that Yang Lijuan et al. Did not consider the level of intracranial pressure.
It is suggested that patients with high intracranial pressure should be given a pillow (7 ~ 8 cm thick and turn over once every 2 hours) after lumbar puncture. The pillow can reduce the postoperative intracranial pressure and indirectly reduce the incidence of cerebral hernia, which is beneficial to the recovery of the disease. Similarly, it is not suitable for patients with low intracranial pressure, and it is recommended to remove the pillow and lie down to avoid further decrease of intracranial pressure. However, in the normal intracranial pressure group, there was no significant difference between postoperative occipital removal and occipital cushion, but occipital cushion could increase the comfort of patients, which was the same as Yang Lijuan’s conclusion.
Therefore, it also reminds us that after lumbar puncture, it is not necessary to [remove the pillow]. Except for patients with low intracranial pressure, it is still recommended to remove the pillow and lie down, other patients can choose the low pillow according to the specific condition to increase the comfort of patients.
Do you have to lie down? Can I use the lateral position?
As Cochrane’s review said, body position also does not affect the occurrence of headache. Even, there is moderate evidence that bed rest lacks significant benefits compared with direct activity after puncture.
There was low quality event for an absence of benefits associated with bed rest compared with immediate mobility on the incident of severe PDPH and modern quality event on the incident of any headache after lumbar puncture.
No matter whether the head is removed or low, the head angle has not changed greatly and there is no difference in theory. In the domestic literature research, there are also comparisons between lying down and lying down on the side. It is believed that the patient’s comfort level can be increased after lying down for 2 hours and then changing to lying down on the side, and the occurrence of pressure ulcer caused by long-term skin compression on the same part can be avoided.
Do you have to lie down on your pillow [4 ~ 6 hours]?
Most reports believe that bed rest for 30 min, 1 h, 2 h, 4 h or 6 h after lumbar puncture has no significant effect on the incidence of headache [7] [8] [9], but the incidence of low back pain in lying down for 30 minutes to 1 hour is significantly lower than that in lying down for 6 hours [10], so it is not necessary to reach [6 hours], and 30 minutes to 1 hour is a good time point.
In clinical practice, if cerebrospinal fluid is extracted by lumbar puncture for testing, only 3 ~ 4 mL of cerebrospinal fluid is generally left for testing, and not much cerebrospinal fluid is released in the whole process.
The production speed of cerebrospinal fluid is about 0.3 mL/min, i.e. 18 mL cerebrospinal fluid is produced within 1 hour, while the circulation absorption speed is slower than before [5]. Does it really take 6 hours to recover? In this regard, foreign countries also have different opinions, and bring many inconveniences to both doctors and patients [6].
With the continuous improvement of puncture needle design, the phenomenon of leakage after puncture has been significantly improved. The original occipital removal and supine lying [to prevent cerebrospinal fluid leakage from causing intracranial hypotension] is also worth discussing again.
