As soon as the baby has a fever, parents are worried. The number on the thermometer makes many parents unable to sleep at two or three o’clock in the morning or even sleepless all night.
Worried that children will burn their brains, and in order to relieve their anxiety, antipyretics have become a magic weapon for many parents.
However, not all antipyretics are suitable for children. Some antipyretics that have serious side effects and should have been blacklisted long ago still exist, just like a tentacle full of venom, which will pull children into danger if you are not careful.
Today, the old editor took stock of several antipyretics that must not be used by children. If the doctor prescribes them, he must firmly say [No].
These four kinds of drugs must not be used by children.

1. Bupleurum injection
Many parents should be familiar with this medicine.
As a star antipyretic that has been used clinically for more than 70 years, Bupleurum injection not only saved countless lives in wartime, but also entered moderns, which was produced in large quantities, after the 1950s.
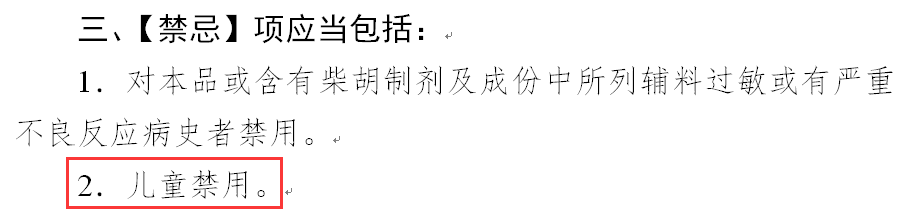
However, Bupleurum injection will lead to many adverse reactions, most of which are allergic reactions, even anaphylactic shock, syncope, etc.
In addition to serious adverse reactions, fatal accidents caused by infusion and intramuscular injection of drugs have also occurred.
A 6-year-old child suffered from epidermolysis bullosa drug eruption due to intramuscular injection of Bupleurum root injection due to fever caused by upper respiratory tract infection. He died after one week of hospitalization after ineffective rescue.
An 11-year-old girl suffered from anaphylactic shock and acute renal failure after intravenous drip of Bupleurum chinense injection 14 mL, and died after ineffective rescue.
Because of frequent accidents, on May 23, 2018, the State Drug Administration officially issued a document to put Bupleurum injection into the “cold palace” banned by children.
2. Analgin
Analgin used to be widely used in clinical practice, but it is still used in some remote areas, some of which are injection and some of which are nasal drops, but it also has serious side effects.
The United States banned Analgin more than 40 years ago, and more than 30 countries such as Japan and Australia have also blacklisted it one after another.
The biggest side effect of analgin is that it may lead to granulocytopenia.
It will greatly reduce the baby’s immunity and increase the probability of infection. For example, a common small cold may bring irreparable damage to the child.
In addition, it may also lead to thrombocytopenic purpura, autoimmune hemolysis, aplastic anemia, urinary system damage, anaphylactic shock and even death.
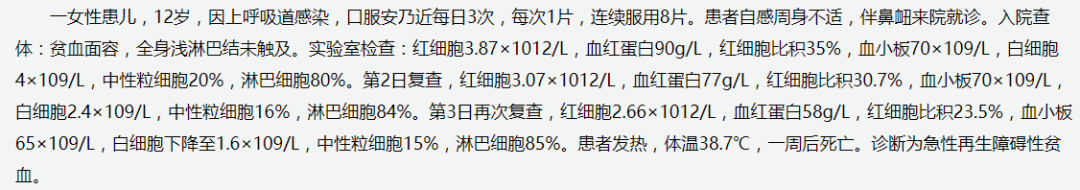
The National Adverse Drug Reaction Monitoring Center once provided a typical case, which made people sad:
A 12-year-old girl, who took analgin orally due to upper respiratory tract infection, was hospitalized for general malaise after taking 8 tablets in a row. A week later, the little girl died and was diagnosed with acute aplastic anemia.
In addition to Analgin, Antongding should also be on guard. The two can be described as “one mother compatriot” and are notorious.

3. Lysine pilin
Lysine pilin is a common type of fever reduction needle. Its advantage is that it can reduce fever quickly, but it can also cause serious adverse reactions.
Children may suffer from convulsion, vomiting and other symptoms after being injected with lysine and pilin, and even coma, which may directly lead to death in severe cases.
This serious adverse reaction is called Wright’s syndrome, with the highest incidence among children under 12 years old.
In addition to lysine, aspirin can also cause Wright’s syndrome.
Therefore, no matter whether the child is still in infancy, can walk or even has gone to school, do not take these two drugs.
4. Nimesulide
Nimesulide was once a popular antipyretic for children, with good effect and quick fever reduction. Many hospitals and clinics like to use it.
However, nimesulide is easy to cause liver and central nervous system damage in children. In China, nimesulide has been banned for children under 12 years old.
If you see a doctor prescribing this medicine, you will refuse it directly without discussion.
There are only two safe antipyretics recommended

I said that antipyretics that cannot be used by children, so what can be used? There is no need for the old editor to repeat it. Many parents should have known long ago that the safest antipyretic is acetaminophen and ibuprofen.
1. Paracetamol
Acetaminophen, also known as paracetamol, was officially used clinically in 1955 and has a clinical use history of more than 60 years. Its safety is very reliable and it is now the most widely used antipyretic and analgesic in the United States.
Acetaminophen is one of the antipyretics recommended by the World Health Organization. Its toxic and side effects are relatively small, and its stimulation to digestive tract is also small. It is more suitable for babies over 3 months old.
However, it is better to pay for acetaminophen with a single ingredient, such as Tylenol, and not to choose compound cold medicine, so as not to take it in excess of the dosage without knowing it and damage the health of children.
2. Ibuprofen
Ibuprofen is another very safe antipyretic for children recommended by the World Health Organization. It was discovered later than acetaminophen and was only synthesized and invented in the 1960s. It has antipyretic, analgesic, anti-inflammatory and uterine muscle contraction effects.
Compared with acetaminophen, ibuprofen has a longer cooling and maintenance effect and is suitable for children over 6 months old (of course, acetaminophen can also be selected). For children under 6 months old, the safety and effectiveness are still uncertain.
It should be noted that ibuprofen is excreted through the liver. If the liver function of the child is not very good, it should also be used carefully.
Knock on the blackboard:
- More than 3 months of children have fever, with acetaminophen (Tylenol) more than 6 months of children have fever, with ibuprofen (Merrill Lynch) less than 3 months of children have fever, it is recommended to see a doctor.
The doses of acetaminophen and ibuprofen are different.

No matter how safe drugs are, there is a prerequisite, that is, to take them correctly, and acetaminophen and ibuprofen are no exception.
Special attention should be paid to the fact that when giving children acetaminophen or ibuprofen, the safest and most effective way is to calculate the dosage according to body weight.
- The minimum dosage of Tylenol was 10 mg/kg and the maximum dosage was 15 mg/kg. The minimum dosage of Merrill Lynch was 5 mg/kg and the maximum dosage was 10 mg/kg.
Children’s fever is a difficulty that every mother will experience. As a smart mother, we should choose the safest medication for our children and accompany them through the most uncomfortable days.
