
The incidence of cardiovascular diseases in China has soared to an outrageous extent. Coronary heart disease, as one of the most influential diseases, has also attracted increasing attention. Especially when celebrities and leaders fall down due to myocardial infarction caused by coronary heart disease, the masses have a more perceptual understanding of coronary heart disease.
As a result, many people began to take antithrombotic drugs (such as aspirin) and 7788 proprietary Chinese medicines after diagnosis of coronary heart disease. However, the use of one drug has been neglected by many patients with coronary heart disease, and that is statins and lipid-lowering drugs.
A large number of them stopped using statins because their blood lipid was normal. In their eyes, statins reduce blood lipid. Why can’t they stop taking drugs when blood lipid is normal?
Hypolipidemic drugs cannot be stopped indiscriminately.
In fact, coronary heart disease patients with normal blood lipid cannot stop using statins without authorization.
Coronary heart disease generally refers to coronary atherosclerotic heart disease, which is the plaque growing on the inner wall of the coronary artery supplying blood to the heart itself. The generation and growth of these plaques are closely related to cholesterol, which can be said to be the raw material for building atherosclerotic plaques, so lowering cholesterol in blood can inhibit the growth of plaques.
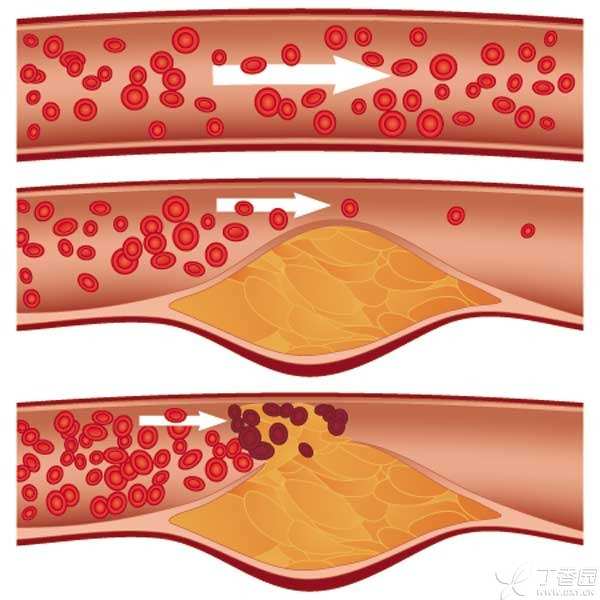
Rupture of atherosclerotic plaque is the cause of vascular occlusion.
But things are not that simple. Myocardial infarction, the number one killer in the coronary heart disease family, is no stranger to everyone. However, many people believe that myocardial infarction is caused by atherosclerotic plaque growing up slowly and then blocking blood vessels. No! !
In fact, the vast majority of myocardial infarction occurs not because the plaque is too large, but because the plaque is broken, inducing acute thrombosis and blocking coronary arteries.
Why did the plaque break? There are many reasons for this, but two of them are very important:
- There is too much fat in atherosclerotic plaque, and the plaque part becomes dumplings with large stuffing and thin skin. Atherosclerotic plaque has inflammatory reaction, and the inner layer of blood vessels surrounding the plaque becomes unstable.
Statins lipid-lowering drugs are not only as simple as lipid-lowering, but also can stabilize plaques and prevent rupture. They are versatile in treating coronary heart disease.
Therefore, it is clear that patients with coronary heart disease, especially patients with unstable angina pectoris and myocardial infarction, or patients with diabetes, should take statins according to the doctor’s advice.

Blood lipid lowering drugs hurt liver?
In addition to not realizing the importance, many patients are also worried about the side effects of statins, the most important of which is liver problems.
At work, I often meet patients who ask me [is this statin very toxic to the liver], and even some patients refuse to take it because they are worried about the liver safety of statin. What’s more, I met a patient with coronary heart disease who stopped using statin a few years ago because the doctor in the hospital told the patient that statin was very toxic to the liver and could not be eaten.
But is this really the case?
The truth is:
- The incidence of statin-related liver damage is about 1.2 per 100,000, Not even [in case]. Because the incidence of liver failure caused by taking statins is only one in 5 million, At present, it is believed that it is caused by the specific constitution of the patient. Statins can be used for nonalcoholic fatty liver disease, chronic liver disease (such as chronic hepatitis B) and compensatory liver cirrhosis. During the process of taking statins, if the liver enzyme increases within 3 times the upper limit, there is no need to stop taking drugs, and the dosage can be reduced or monitored continuously.
Statins are not recommended for patients with the following conditions:
Active liver disease, persistent liver enzyme elevation of unknown causes, liver enzyme elevation of any cause exceeding 3 times the upper limit of normal value, decompensated liver cirrhosis, acute liver failure.
Finally, in combination with relevant guidelines and personal experience, I suggest that patients should check their liver function before and one month after taking statins, and then every 6-12 months to prevent serious side effects.
For those who should take statins, statins are definitely a drug with more advantages than disadvantages. I hope this article can eliminate most people’s unnecessary worries about statins and better standardize medication.
The article was reprinted by Clove Garden authorized by the author.
