Introduction: Obsessive-compulsive Behavior and Obsessive-compulsive Disorder Patients
Do you repeatedly check whether the doors and windows are closed in your daily life? Do you sometimes know clearly that the car door is locked, but you still feel uneasy and need to go back and check it again? Do you feel that you should follow a certain sequence or pattern when dressing, cleaning, eating, walking and sleeping, otherwise you will be upset and anxious?
At this time, perhaps you will ask yourself, do I have obsessive-compulsive disorder? Obsessive-compulsive disorder is a type of neurosis. It is mainly composed of obsessive-compulsive concept and/or obsessive-compulsive behavior. It is characterized by the coexistence of conscious self-compulsive and anti-compulsive. The strong conflict between the two makes patients feel anxious and painful. Patients know that obsessive-compulsive concept or behavior comes from themselves, but they violate their own wishes. Although they try their best to get rid of it, it is of no help.
Obsessive-compulsive disorder is the fourth common mental disorder after depression, alcohol/drug abuse and social phobia. In the community epidemiological survey, the lifelong prevalence rate of obsessive-compulsive disorder is 1.6%. The severity of obsessive-compulsive disorder varies from person to person.
When obsessive-compulsive disorder occurs in childhood or adolescence, Teenagers may avoid interacting with their peers, Or become unable to live independently, The World Health Organization (WHO) has listed obsessive-compulsive disorder as one of the top ten diseases that seriously affect people’s quality of life and income. When individuals suffer from obsessive-compulsive disorder, they may choose to hide their obsessive-compulsive symptoms from their family members, relatives, friends or colleagues, which may lead to interpersonal problems and affect their ability to work or study.
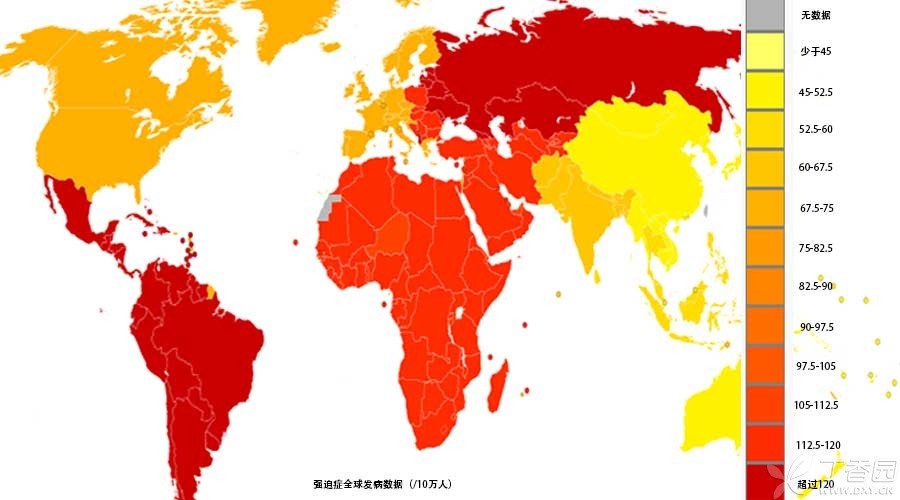
Epidemiology: 50 million!
Obsessive-compulsive disorder has become a global problem. It is estimated that there are at least 50 million obsessive-compulsive disorder patients in the world, and the incidence rate is also increasing in recent years, although social and cultural factors will also affect the occurrence of obsessive-compulsive disorder.
For example, religious ceremonies that are common in some countries, In addition, China’s awareness of taboos should not be ignored. In an increasingly fierce modern society, many successful people do not let go of every detail of their products, strive to be almost perfect and maintain their advantages in competition. However, this trait is also one of the common personality characteristics of obsessive-compulsive disorder.
Epidemiological surveys around the world show that the prevalence rate of obsessive-compulsive disorder is equivalent between men and women, but women are more likely to wash their hands by force. Men are more likely to have compulsive sex (or sexual addiction, in which patients are unconsciously eager to have sex with others.), which is considered characteristic for some specific figures, and slow to move due to ritual movements. (Editor’s Note: There may be cultural differences)
For the average onset age of obsessive-compulsive disorder, Men tend to be at the end of puberty, Women are just about 20 years old, however, obsessive-compulsive disorder can also occur in the elderly, who have a long history but have not been diagnosed or have most clinical manifestations that conform to obsessive-compulsive disorder in a short period of time. Children and adolescents can also suffer from obsessive-compulsive disorder, with the prevalence rate between 5 and 15 years old being about 0.25%, and some manifestations similar to adult obsessive-compulsive disorder.
However, there are differences in different stages of development. For example, compared with children, in adolescence, sexual relations or religious compulsion are more common. Young people are more afraid of the death of their parents than adults. Children are less likely to have sudden obsessive-compulsive symptoms and intermittent attacks, and have tic disorders, hyperactivity or dance-like movements.
The causes of the disease are various.
Based on twins and genome-wide linkage studies, obsessive-compulsive disorder has genetic susceptibility. Some studies have reported that the same disease rate between obsessive-compulsive disorder patients and their parents is 5%-7%, the disease risk of obsessive-compulsive disorder in first-degree relatives is 3%-5%, and about 40% of monozygotic twins and 30% of dizygotic twins have certain obsessive-compulsive symptoms.
It also includes psychosocial factors, including sexual abuse, emotional neglect, social isolation, ridicule or bullying, etc. Psychological factors include absoluteness, high sense of responsibility, perfectionism, exaggerated imagination of danger, and personality characteristics such as introversion, timidity, seriousness, indecision, seriousness, rigidity and conformity.
There are also stress factors before and after delivery, such as postpartum obsessive-compulsive disorder, which will constantly worry about whether they will hurt, abuse or not take good care of their baby.
At present, there is little evidence for physiology and pathology of obsessive-compulsive disorder. According to some known research results, obsessive-compulsive disorder may be related to 5-HT neurotransmitter system. It is also found that some pathological changes of the brain can also lead to obsessive-compulsive disorder, such as some brain trauma, epilepsy, diseases affecting basal ganglia, etc. Some obsessive-compulsive disorder patients also have neurological soft signs.
In recent years, brain structural and functional imaging studies have suggested that the volume of gray matter in the head of unilateral or bilateral caudate nucleus in some patients is reduced, while the resting metabolic activity of medial prefrontal orbital cortex and basal ganglia is increased, and metabolism is decreased after effective drugs or psychotherapy, suggesting that the neural loop activity of medial prefrontal orbital cortex and basal ganglia is enhanced.
In addition, there are reports of drug-induced anti-obsessive-compulsive disorder, Mainly antipsychotic drugs, The notable feature of drug-induced obsessive-compulsive disorder is that, After reducing the dosage of antipsychotic drugs or stopping drugs, obsessive-compulsive symptoms can be gradually relieved or disappeared. Especially in the new generation of antipsychotic drugs, such as clozapine, as the first choice drug for the treatment of refractory schizophrenia, its curative effect is worthy of affirmation, but the obsessive-compulsive symptoms caused by clozapine are also the most common. At the same time, olanzapine, risperidone and so on have also been reported.
